You’re reading the web version of Health Care Inc., STAT’s weekly newsletter following the flow of money in medicine. Sign up to get it in your inbox every Monday.
Hello, you spry bunch. We’re coming to you on a Tuesday after yesterday’s holiday. What are you looking to read more about as the year winds down? Let us know: [email protected].
UnitedHealthcare’s new prior authorizations
Adobe
Getting physical, occupational, and speech therapy is about to get a lot more burdensome for people who have a UnitedHealthcare Medicare Advantage plan.
A friendly neighborhood tipster alerted me to new prior authorization rules put out by UnitedHealthcare, the insurance arm of UnitedHealth Group. As of Sept. 1, Medicare Advantage members who need PT, OT, or ST in a physician’s office or an outpatient hospital clinic will need to get approval from UnitedHealthcare.
Getting PT, OT, and ST in your home is cheaper than getting them in an outpatient clinic, but that’s not necessarily feasible for everyone. This will create headaches not just for UnitedHealthcare MA enrollees, but also the therapists who will have to file more paperwork to justify the sessions.
There’s another financial angle here for UnitedHealth, beyond potentially paying out fewer claims for therapists. UnitedHealth is also directing more of these services to itself. (Sound familiar?) People who get these services in their house are excluded from the prior authorization requirements — UnitedHealth just so happens to own a bunch of firms that offer PT, OT, and ST at home. Read UnitedHealthcare’s new prior authorization rules here.
Live from Boston!
STAT’s annual Summit is this week, so if you’re in Boston, come check it out and say hi. (It’s being held virtually, too.)
My colleague Tara Bannow and I will be moderating sessions that may pique your interest. Tara will be on stage with three of the physicians who spoke with us for our ongoing Health Care’s Colossus series about UnitedHealth. And I’ll be chatting with former CMS administrator Don Berwick about Medicare Advantage and other important ways to think about Medicare post-election. The entire agenda is here.
A conservative judge’s war on the False Claims Act
For the first time, a Trump-appointed judge in Florida ruled that the whistleblower provisions of the False Claims Act are unconstitutional, Tara reports.
The finding could lay the groundwork for similar challenges to the law. The FCA is the government’s number one tool for rooting out fraud in public health care programs, and it relies chiefly on private citizens filing whistleblower claims that the government can join. The government recovered about $2.7 billion under the law in fiscal 2023.
In her ruling dismissing a case alleging Medicare Advantage fraud, federal district judge Kathryn Kimball Mizelle argued the FCA’s whistleblower provisions are unconstitutional because they essentially make whistleblowers appointees of the executive branch, despite there being no appointment process. Even though Mizelle is a conservative judge, Max Voldman, an attorney who represents whistleblowers, told Tara he doesn’t think opinions on the FCA cut neatly across political lines.
Voldman expects Mizelle’s ruling to give rise to more such FCA challenges, even though he thinks this one will crumble on appeal. “This is, as far as I know, the first court to take this position as opposed to dozens on the other side,” he told Tara. Read the full ruling.
$25,572
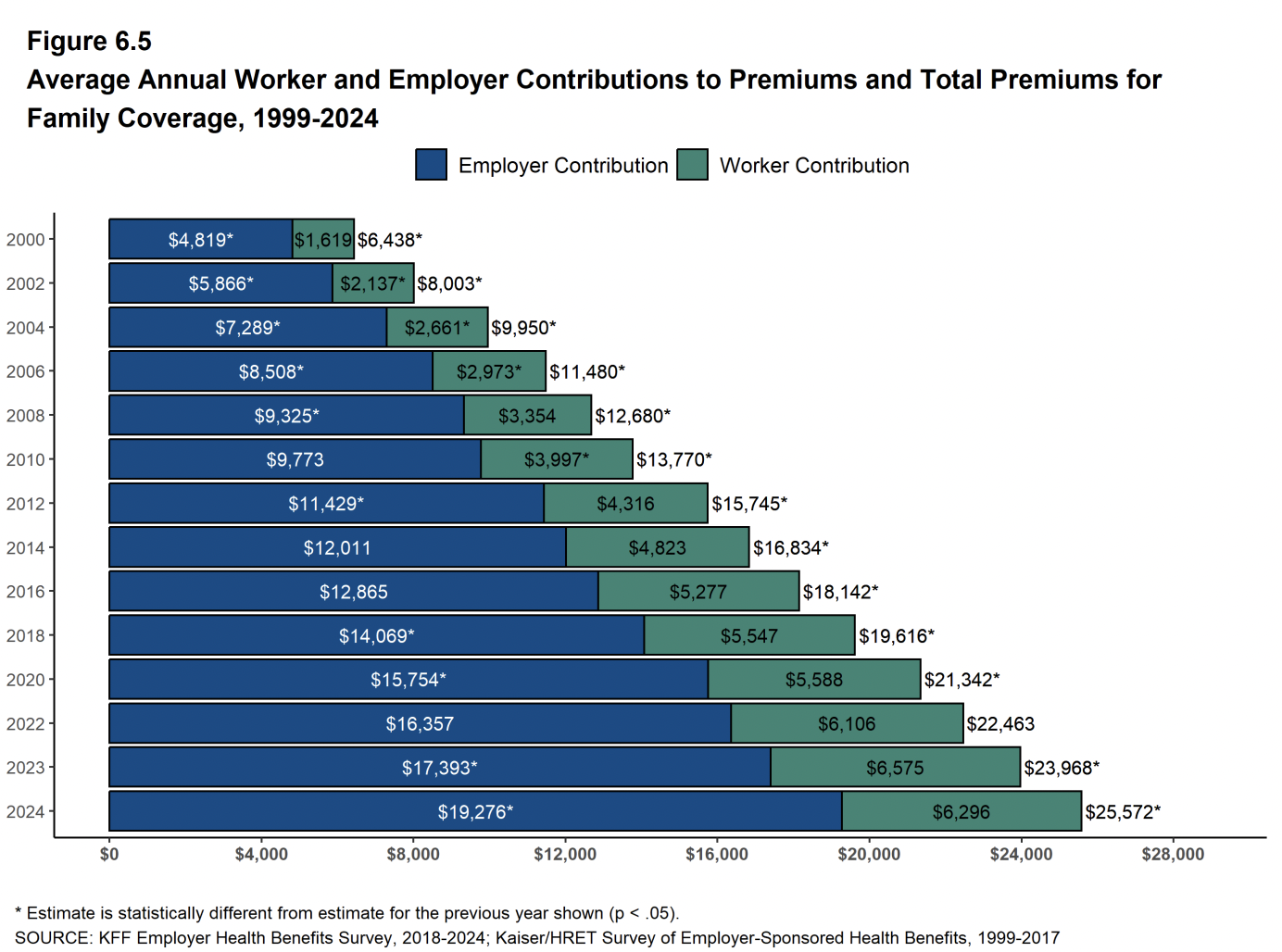
Workers are paying less out of their paychecks for their health insurance (for both single and family coverage) for the first time in the 25 years health policy nonprofit KFF has surveyed employer health coverage. The latest report is here. However — and this is a massive however — employers are shelling out a lot more on the back end. That translates to family coverage now costing more than $25,000 annually on average.
That’s still your compensation getting shoveled into health insurance instead of wages. Enjoy the pay cut.
Star-dudded
The Biden administration officially released the star ratings for 2025 Medicare Advantage plans last Friday. There were few surprises considering how Humana and UnitedHealth already signaled tough sledding for the industry.
Getting at least four out of five stars is the target of every insurer because that’s when a 5% bonus payment kicks in. And it’s clear after several methodological changes by the government, clearing the four-star threshold is not as big of a cakewalk as it used to be.
The percentage of Medicare Advantage enrollees in plans with at least four stars:
2022: 90%
2023: 72%
2024: 76%
2025: 62%
Industry odds and ends
Welcome to Q3 earnings season. UnitedHealth kicks things off today, followed by Elevance Health on Thursday morning, and Intuitive Surgical on Thursday afternoon. Nonprofit hospital system Trinity Health also is holding its annual “investor call” (remember, it’s a nonprofit!) on Wednesday afternoon.
The “Big 3” PBMs are following in the footsteps of big tech companies that are extremely mad at Lina Khan. Last week, they filed legal documents demanding that Khan and the two other Democratic FTC commissioners be removed from the FTC’s lawsuit against them, claiming they’re biased against them. For example, they don’t like how she appeared at a conference where attendees called PBMs “bloodsuckers.” Read more (which includes links to the filings for each company).
Experts who sit on the Medicare Payment Advisory Commission expressed concerns about the perks offered by Medicare Advantage plans, Cheryl Clark of MedPage Today reports. “Beneficiaries are attracted to these extra benefits, and may join Medicare Advantage because of them, and yet the evidence kind of shows that use of these extra benefits is low,” one of the MedPAC commissioners said at a meeting last week.
Some big companies like JPMorgan Chase are returning to the days of on-site clinics, but it may be creating “the unintended consequence of exacerbating a two-tiered system,” Alex Olgin and Dan Gorenstein report for Tradeoffs.
Ascension officially completed its transaction with Henry Ford Health to create a multi-hospital joint venture in Michigan. But a bondholder notice has some unclear language about the deal’s details. Ascension threw in its hospitals, and “in exchange Ascension Health received an interest in [Henry Ford Health System].” An ownership interest in the joint venture, or an ownership interest in the entire Henry Ford Health System? An Ascension spokesperson did little to clarify, saying the board members of the new partnership “have voting rights that directly correspond to the percentage of the contributed value of their assets to the JV agreement.”
The Meme Ward

Thank you to everyone who has reached out to Casey Ross and me on the Loeb Award. We’re beyond honored. A special kudos to all of STAT, including my colleagues who were finalists for the “Obesity Revolution” series. Several of them above — Isa Cueto, Matt Herper, Laura Chang, Gideon Gil, and Elaine Chen, who snapped the photo — inadvertently created a new meme format







