The body naturally defends a certain weight range. When you reduce calories too sharply, energy expenditure drops and hunger hormones rise. This adaptive response makes crash diets ineffective. Sustainable plans respect biology rather than fighting it.
The National Institutes of Health (NIH) emphasizes that metabolism, sleep, and environment all influence weight beyond calorie counting.
At Valley Medical Weight Loss, we guide patients through gradual changes that the body can accept. Nutrient-dense meals, adequate protein, hydration, and consistent routines form the foundation of every plan.
Genetics and Epigenetics Influence Metabolism
Family history can shape metabolism, appetite, and fat distribution. Genetics influence how easily the body stores fat or feels satisfied after eating. Yet, genes are not destiny. Epigenetics, or how behaviors and environment affect gene expression, means lifestyle can still change outcomes.
Research shows that early-life stress, poor sleep, or high intake of ultra-processed foods can “program” metabolism toward easier weight gain. The CDC notes that these influences are modifiable through better sleep, stress management, and nutrition.
When patients understand this, they stop blaming themselves and start focusing on the factors they can control.
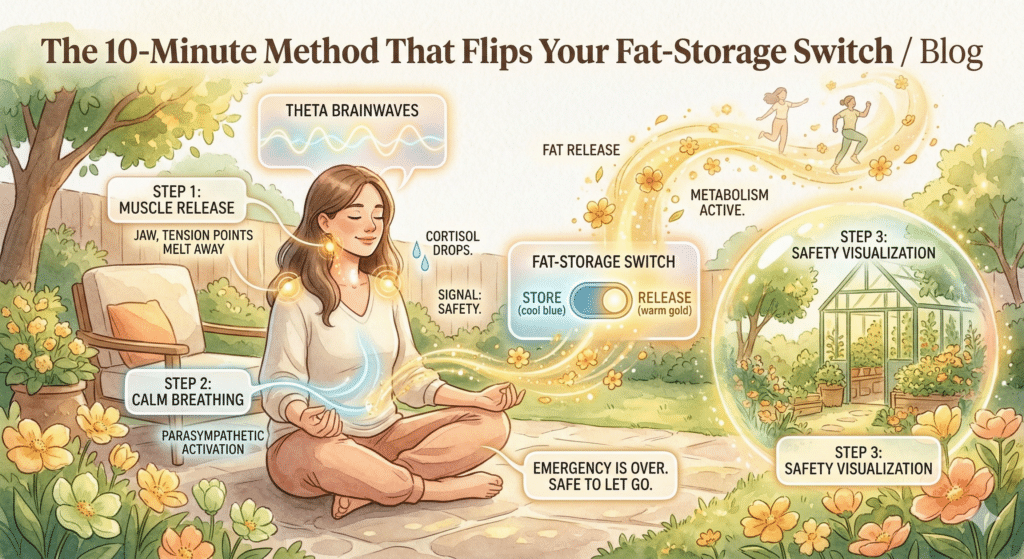
Sleep and Stress Affect Hunger and Fat Storage
Lack of sleep raises ghrelin, the hunger hormone, and lowers leptin, the satiety hormone. Combined with chronic stress, elevated cortisol can increase abdominal fat and reduce impulse control. According to the CDC, short sleep duration and stress are linked to higher obesity risk.
In our program, sleep is treated as a core behavior, not an afterthought. We help patients set consistent bedtimes, reduce screen exposure, and adjust caffeine intake. These small habits can rebalance hunger hormones and improve appetite control within weeks.
Medications and Health Conditions Matter
Several common prescriptions can cause weight changes by altering metabolism, appetite, or fluid balance. Examples include certain antidepressants, corticosteroids, insulin, and antipsychotics. Health conditions like hypothyroidism, polycystic ovary syndrome (PCOS), or Cushing’s syndrome also play a role (CDC Obesity Risk Factors).
At Valley Medical Weight Loss, every intake review includes a full medication history. The goal is not to blame the medicine but to adjust the plan around real-world physiology.
Culture and Environment Influence Eating Habits
Food traditions are powerful. Many of us grew up on rice-based meals, breads, tortillas, or family recipes rich in nostalgia. The challenge is not culture itself but the modern environment that surrounds us. Ultra-processed foods, oversized portions, and constant snacking all create obstacles.
The National Center for Biotechnology Information (NCBI) notes that environmental and social drivers are among the strongest influences on obesity.
In practice, we help patients preserve flavors and traditions while improving proportions and preparation. We encourage small swaps, such as:
- More vegetables and protein
- Smaller portions of refined starches
- Spices, herbs, and citrus for flavor instead of added sugar
When nutrition fits your lifestyle, it lasts.
Motivation Is Often the Missing Ingredient
Motivation is not a constant. It fluctuates, especially when people try to lose weight for external reasons rather than internal goals. The best outcomes occur when structure and accountability carry you through low-motivation phases.
Recent CDC communications reinforce that obesity is not a moral failing. It is the result of many interacting forces including genes, sleep, medication, stress, and environment. Recognizing this helps replace shame with science.